It’s not uncommon to experience gum pain, swelling, or irritation years after having a wisdom tooth extracted. Even though the tooth is gone, the area where it used to be can act up long after the initial healing period. There are a few potential reasons why you may have lingering discomfort at the site of an old wisdom tooth extraction.
Common Causes of Pain After Wisdom Tooth Removal
Infection
One of the most common causes of pain years after wisdom tooth removal is a low-grade infection in the bone or soft tissues around the extraction site. When a wisdom tooth is extracted, it leaves behind an empty socket in the bone which eventually fills in with new bone and tissue.
However, small particles of the tooth or gum tissue can be left behind which can lead to bacterial growth and chronic inflammation. Typical signs of infection include:
- Throbbing, aching, or sharp pain at the extraction site
- Redness, swelling, or discharge of pus from the gums
- Bad breath or bad taste in the mouth
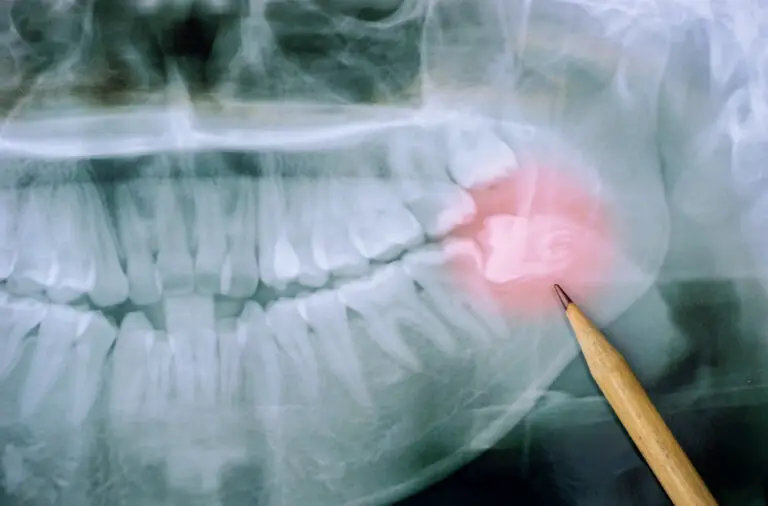
An x-ray may be needed to check for left behind tooth fragments or other foreign material that could be causing recurrent infections. Antibiotics or dental surgery may be necessary to clear a stubborn tooth socket infection.
The most common bacteria involved in these post-extraction infections are viridans streptococci, Fusobacterium, Bacteroides, Peptostreptococcus, and Prevotella. These bacteria naturally reside in the oral cavity but can proliferate and cause problems in the empty socket or areas of gum irritation after wisdom tooth removal. Infection can also spread to adjacent teeth, the jaw bone (osteomyelitis), neck spaces, or even systemically in rare cases of severely uncontrolled infections.
Diabetes, smoking, poor nutrition, and immunosuppression increase susceptibility to prolonged gum infections after extraction. Meticulous at-home oral hygiene and regular dental cleanings help prevent opportunistic bacterial growth. But once established, antibiotics like penicillin, clindamycin, or metronidazole are usually needed to eliminate the stubborn infection.
Dry Socket
Dry socket (alveolar osteitis) occurs when the blood clot at the extraction site fails to form properly or gets dislodged too soon after the tooth removal. This exposes the underlying bone and nerves. Dry socket usually causes severe, radiating pain starting a few days after having the tooth pulled.
While dry socket most often happens within the first week after wisdom tooth extraction, it can occasionally happen years later if food or debris gets impacted in the empty socket. The pain won’t resolve until new tissue can form over the bone. Rinsing with warm salt water and getting a medicated dressing packed into the socket by a dentist can help ease dry socket discomfort.
Dry socket happens when increased fibrinolysis breaks down the normal clot too early. Bacterial contamination can also prevent clot formation and retention. Smoking, birth control, trauma to the socket, and pre-existing infections increase dry socket risk. Packing the socket with zinc oxide eugenol paste provides pain relief and protects the underlying bone until healing can occur.
Nerve Damage

Lingering pain after wisdom tooth removal may signal injury to the lingual or inferior alveolar nerves during the extraction. These nerves provide sensation to the tongue, lower teeth, chin, and lower lip on the affected side.
Nerve damage during oral surgery is rare but can cause painful neuropathy symptoms like shooting, burning pain or numbness years later. This nerve pain is often worse with chewing or touch. If nerve injury is suspected, your dentist may refer you to an oral surgeon or neurologist for evaluation and treatment.
The lingual and inferior alveolar nerves are at risk during lower wisdom tooth removal since they run just under the gums in that area. Excessive force, stretching, clamping, or lacerations can damage the nerves. Most post-op nerve pain resolves within a few weeks to months, but severe injuries cause permanent paraesthesia. Gentle massage, pain medications, desensitizing toothpaste, and time usually help manage discomfort until the nerves can hopefully heal.
Scar Tissue Formation
The body’s natural healing process after wisdom tooth extraction involves formation of scar tissue and bone remodeling over the socket. Sometimes this can result in thicker, overgrown scar tissue that is more prone to irritation and recurring pain with chewing years later. Food particles and debris can also get trapped in this fibrous gum tissue and provoke inflammation.
Massaging the area with a warm washcloth and using an oral irrigator on a low setting can help break up scar tissue over the extraction site and relieve discomfort. More extensive surgery to remove scar tissue may be warranted in severe cases.
Scar tissue is part of normal healing, but some people form exuberant granulation tissue which is hyper-sensitive and easily damaged. Genetics, oral hygiene, and habits like chewing on the wound margins impact scar formation. Manual debridement and medicated dressings help manage troublesome scar tissue. In refractory cases, steroid injections or surgery removes the overgrown tissue.
Jaw Joint Issues (TMJ)
Pain at the site of wisdom tooth removal may actually be referred discomfort from the temporomandibular joint (TMJ). TMJ connects the lower jaw bone to the skull. Having a wisdom tooth extracted can sometimes exacerbate or lead to TMJ problems like arthritis, dislocation, or disc derangement which then causes chronic jaw pain.
Seeing a TMJ specialist for splint therapy or physical therapy on the jaw muscles may be needed for TMJ-related wisdom tooth removal pain. Botox injections and surgery are other options for recalcitrant TMJ disorders.
The temporomandibular joint and associated muscles help open and close the mouth. Wisdom tooth removal impacts the bite which can lead to imbalance in jaw movement and loading forces. TMJ inflammation develops over time, so symptoms might not be noticeable for months or years after an extraction. Conservative treatments involve NSAIDs, soft diets, physical therapy, and bite splints. Surgery like disc repositioning, orthognathics, or total joint reconstruction may be warranted for severe impingement, arthritis, or anatomical abnormalities causing protracted pain.
When to Seek Evaluation for Lingering Pain After Tooth Extraction

You should make an appointment to see your dentist if you have:
- Severe, unrelenting pain more than a week after wisdom tooth removal
- Fever, chills, nausea, or fatigue – possible signs of infection
- New or worsening numbness in your tongue, lip or chin – may indicate nerve injury
- Pain, stiffness or popping when opening your jaw – could be TMJ issues
- Bad breath, taste or gum swelling – suggests inflammation or debris trapping
Don’t delay getting gum pain near your wisdom tooth socket evaluated. Left untreated, infection can spread and nerve injuries usually don’t improve over time. Early intervention gives you the best chance for successful resolution. Keep monitoring for signs the problem is getting worse and seek emergency care if you develop swallowing difficulties or progressive swelling in your jaw, neck, or face as these can indicate a spreading infection.
Diagnosis of Lingering Wisdom Tooth Extraction Pain
There are a few different methods your dentist may use to figure out what’s causing discomfort years after having a wisdom tooth pulled:
Clinical Examination
Careful visual inspection and palpation of the gums over the extraction site can find signs of infection like swelling and discharge. Testing for loose teeth or cracks helps identify referred pain. Examining gum recession and scarring reveals excessive fibrous tissue buildup. Pressing on the temporomandibular joint while opening and closing the mouth assesses for clicking, popping or grinding that could indicate TMJ disorders. Checking lip and tongue sensation detects possible nerve injury.
Dental Imaging
X-rays, CT scans or CBCT imaging allow detailed visualization of the extraction site and surrounding bone. Your dentist looks for retained tooth fragments, foreign bodies, or bony abnormalities possibly linked to your pain. Imaging also identifies infection, bone loss, cysts or tumors. Special TMJ films help evaluate joint integrity and position too.
Bacterial Culture
Collecting a small sample of fluid or tissue from your painful gum and sending for laboratory culture identifies pathogenic bacteria if infection is the culprit. This pinpoints the correct antibiotic for treatment. Anaerobic cultures may be needed to isolate the fastidious oral bacteria often involved.
Allergy Testing
Rarely, some dental materials or antibiotics used during extraction provoke delayed allergic responses even years later. Allergy testing and elimination trials uncover sensitivity contributing to chronic localized inflammation after wisdom tooth removal.
Treatments for Lingering Pain After Wisdom Tooth Removal

The treatment your dentist recommends depends on the specific cause identified, but may include:
Medications
- Antibiotics – Prescribed for 1-2 weeks to clear suspected bacterial infections. May require repeated or long-term courses for chronic infection.
- Oral steroids – Help reduce swelling and inflammation in the area. Useful for acute flare ups or while waiting for antibiotics to take effect.
- NSAIDs – Over-the-counter anti-inflammatories like ibuprofen relieve discomfort and pain. Should be taken regularly for best results.
- Nerve pain medications – Tricyclic antidepressants, gabapentin, or carbamazepine prescribed for neuropathic nerve symptoms.
- Muscle relaxants – Help ease TMJ spasms and tension contributing to pain.
Debridement
Removing debris, food, or granulation tissue from the socket using hand tools or ultrasonic scalers provides relief if trapped material is irritating the area.
Wisdom Tooth Fragment Removal
If left-behind tooth pieces are found, your dentist surgically opens the gum and carefully takes them out. This removes the infection source and allows the tissue to heal.
Alveoloplasty
Smoothing rough, protruding bone edges around the extraction site through contouring or grafting reduces gum irritation. Useful when bone spicules have formed.
Physical Therapy
Stretching exercises, massage, warm compresses, cold therapy, and ultrasound applied to the jaw joint provide relief for TMJ-related wisdom tooth pain. Can be done at home or with a physical therapist.
TMJ Injection
Injecting anesthetics, steroids or other anti-inflammatory agents directly into the temporomandibular joint calms inflammation and discomfort. Often provides immediate, short-term improvement.
TMJ Surgery
Operations like arthroplasty, disc repositioning or total joint replacement are options for advanced TMJ arthritis, impingement or damage causing persistent wisdom tooth removal pain.
Frequently Asked Questions About Pain After Wisdom Tooth Extraction
How long after wisdom tooth removal can you still have pain?
It’s typical to have pain for up to 1 week after wisdom tooth extraction as part of normal healing. Occasional, minimal discomfort may linger for several more weeks. Pain continuing past 2 months likely indicates complications like infection, nerve injury or TMJ issues. Contact your dentist if significant pain persists beyond 10-14 days.
Can wisdom tooth removal cause TMJ?
Wisdom tooth extraction doesn’t directly cause TMJ disorders, but may worsen or uncover pre-existing TMJ problems. The trauma of tooth removal and altered chewing patterns post-extraction can exacerbate joint inflammation. TMJ symptoms may not become noticeable until months or years later. Have your TMJ evaluated if discomfort arises long after extraction.
What helps with dry socket pain?
Dry socket discomfort usually peaks in severity 3-5 days after extraction. Gently rinsing with warm salt water helps keep debris clear. Medicated numbing gels applied to the area provide some pain relief. Having your dentist pack the socket with gauze soaked in eugenol offers more significant pain relief until healing progresses. Avoid disturbing the clot with forceful oral rinsing during initial recovery.
Can a wisdom tooth grow back after extraction?
Wisdom teeth removed in their entirety will not grow back. However, if tooth fragments get left behind, they can become infected and mimic a wisdom tooth growing back. Surgical removal of left-behind pieces stops this pain. Wisdom tooth roots left in place can also sometimes regenerate into a painful, partially formed tooth structure requiring extraction.
When should you see a doctor for wisdom tooth pain?
See your dentist promptly if you have severe, unrelenting wisdom tooth pain that persists or worsens more than 1 week after extraction. Also seek urgent evaluation for pus discharge, fever, swallowing problems or progressive numbness in your tongue, lip or chin which could indicate a serious complication requires emergency treatment. Don’t delay getting treatment.
Outlook for Lingering Wisdom Tooth Extraction Pain
The prognosis depends on the particular cause of your symptoms, but with proper treatment, discomfort after wisdom tooth removal can often be eliminated.
- Infections typically resolve fully with antibiotics and drainage.
- Removing left-behind tooth fragments stops that source of recurrence.
- Dry socket pain subsides once the socket refills with tissue.
- TMJ therapy can effectively manage inflammation and dysfunction.
- Mild nerve injuries may improve over time but severe damage is often permanent.
With your dentist’s help identifying and properly treating the underlying problem, you can hopefully find relief from wisdom tooth extraction pain, even years later. Consistent follow-up is important to ensure any complications are fully resolved or controlled. Catching issues early leads to better outcomes.