Gum pain, also referred to as gingival pain, is an irritation or soreness affecting the soft tissues surrounding and supporting the teeth. It is commonly caused by gingivitis or other gum diseases, but may also result from injury, oral ulcers, dry mouth, or pregnancy hormonal changes. Gum pain ranges from mild tenderness to sharp pain and can make eating, drinking, brushing teeth, flossing and talking uncomfortable. Understanding the various causes of gum pain and utilizing home remedies and professional dental treatments can help relieve symptoms and address underlying conditions.
Causes and Risk Factors for Gum Pain
A number of different conditions can trigger irritation and inflammation leading to gum pain:
Gingivitis
Gingivitis is an early form of gum disease caused by plaque buildup along and under the gumline. Plaque is a sticky film containing bacteria, food debris and saliva minerals. Without thorough daily brushing and flossing, plaque accumulates and the bacteria infect the gums. This causes redness, swelling, sensitivity and potential bleeding. Mild to moderate gum pain is common with gingivitis. If left untreated, gingivitis may advance to more serious gum disease and periodontal damage.
Periodontitis
When gingivitis is allowed to progress, periodontitis can develop. This severe form of gum disease occurs when plaque spreads deep below the gumline into the periodontal pockets surrounding the tooth roots and jawbone. Toxins from plaque bacteria not only inflame the gums but also the underlying bone tissue. As the infection destroys gum tissue and bone, the pockets deepen and teeth can become loose or fall out. Periodontitis sufferers often experience acute gum pain, especially when chewing or eating.
Traumatic Injury
Direct trauma to the gums through biting the cheek, improper flossing technique, sports injuries or dental procedures can tear or cut the soft gum tissues. This can expose nerve endings and cause significant pain. Cuts and abrasions require good oral hygiene to keep the area clean while healing. Dentists may apply medication to numb pain and prevent infection.
Mouth Sores
Oral ulcers affecting the gums including canker sores, fever blisters or cold sores outbreaks, are another common source of gum pain. Certain foods, oral hygiene habits, or irritation can aggravate these sores and make them quite painful until they heal. Those with autoimmune disorders are at increased risk for recurring mouth ulcers.
Abscessed Tooth
An abscess occurs when infection spreads to the root and pulp of the tooth. Abscesses typically cause throbbing toothache but the pus buildup can also put pressure on and inflame the gums. Gum swelling, sensitivity, and pain often accompany a dental abscess, especially as the infection progresses. Abscesses require antibiotic treatment and possibly root canal therapy or extraction to clear out the infection.
Dry Mouth
Insufficient saliva flow or dry mouth syndrome can affect the moisture level and lubrication inside the mouth. Chronic dry mouth tends to make the oral tissues, including gums, more prone to friction, irritation and inflammation. The lack of saliva benefits also increases risk for cavities and gum disease. Certain medications, autoimmune conditions, radiation therapy to the head/neck and habits like breathing through the mouth can cause xerostomia or dry mouth.
Pregnancy Gingivitis
The hormonal fluctuations during pregnancy can increase blood circulation and sensitivity within the gums. Pregnancy gingivitis is quite common, especially during the 2nd and 3rd trimesters, and involves swollen, tender gums that are more likely to bleed when brushing and flossing. Most cases resolve postpartum without treatment but good oral hygiene and regular dental cleanings are recommended during pregnancy to prevent more severe problems.
Medication Side Effects
Some prescription and over-the-counter medications have side effects that impact gum health and lead to pain. Oral contraceptives, antidepressants, blood pressure medications, and more can increase likelihood for dry mouth and gum inflammation. Other drugs cause abnormal gum overgrowth or enlargement that is prone to bleeding and tenderness when brushing teeth. Patients should be aware of oral health risks associated with their medications.
Grinding and Clenching
Excessive teeth grinding or clenching, especially during sleep, can traumatize the gum tissues and temporomandibular joint. This chronic trauma exacerbates gum sensitivity and is linked to headaches, tooth wear, fractures, and loosening. Night guards help cushion the impact from bruxism and minimize gum irritation. Managing stress can also reduce grinding habits.
Symptoms of Gum Pain

Signs that may indicate gum pain:
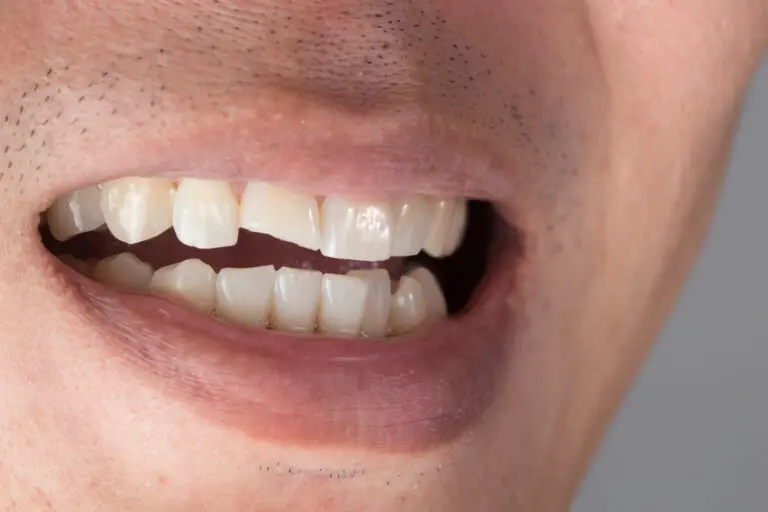
- Sensitive, painful or sore gums
- Red, swollen or inflamed gums
- Bleeding when brushing or flossing
- Receding gumline and exposed tooth roots
- Spaces developing between teeth
- Pus around teeth and gums
- Persistent bad breath or bad taste
- Changes or shifting in tooth alignment
- Loose teeth, fillings or dental crowns
Gum pain can be acute and severe or mild, chronic and intermittent depending on the cause. The degree of pain often relates to the extent of inflammation and infection. Abscesses, advanced periodontitis, severe gingivitis or major trauma usually involve more extreme pain. Milder gum irritation may only cause twinges of discomfort when chewing or occasional bleeding. But any significant gum pain lasting more than a day or two warrants having your dentist evaluate your oral health.
Diagnosing the Cause of Gum Pain
Dentists have a number of methods available to determine the underlying reason for gum pain:
- Reviewing medical and dental history – Past gum disease, trauma, oral infections, medications taken, chronic illness and symptoms experienced can point to likely culprits.
- Oral examination – Checking for visual signs of plaque buildup, swollen gums, canker sores, cracked/worn teeth, etc. allows dentists to assess the health of gums and other oral tissues.
- X-rays and imaging – Dental radiographs, CT scans and MRI imaging help dentists detect issues below the surface such as periodontal bone loss, tooth decay, cysts or abscessed tooth roots.
- Measuring periodontal pockets – A periodontal probe is used to measure pocket depth around each tooth. Deeper pockets often indicate active gum disease.
- Testing tooth, gum and bone stability – Gentle probing around teeth identifies mobile teeth or soft, deteriorating bone.
- Bite and occlusion evaluation – Assessing the contact between top and bottom teeth while biting and chewing checks for imbalance or excessive grinding forces.
- Saliva testing – Analyzing saliva flow and content can reveal dry mouth or high levels of plaque bacteria.
Thorough diagnosis identifies if inflammation, infection, trauma, tissue irritation, or some combination of problems is responsible for the gum pain. This allows selection of appropriate treatment.
Professional Treatment Options for Painful Gums
Depending on the diagnosis, dentists may utilize the following treatments to manage gum pain:
Nonsurgical Therapies
- Professional dental cleaning – Removing built-up calculus (tartar), plaque and bacteria from above and below the gumline can treat gingivitis and sometimes early periodontitis.
- Scaling and root planing – Deep cleaning process to clean microscopic bacteria and toxins from periodontal pockets and smooth root surfaces. This can help pockets heal and shrink.
- Medications (antimicrobials, antibiotics, antiseptics) – Antibacterial and anti-inflammatory drugs treat gingivitis and periodontal infections. Medicated chip treatments slowly release medication into periodontal pockets.
- Laser therapy – Lasers help reduce inflammation and bacterial levels around gum tissues and periodontal pockets.
- Oral hygiene instruction – Dentists emphasize proper brushing, flossing, diet and other gum care techniques based on the individual’s oral health needs and deficits.
Surgical Therapies
- Gum surgery (gingivectomy, flap procedure, graft) – Involves lifting gum tissue flaps to access and remove infected tissue, then smoothing and suturing the gums closer to the healthy underlying bone. May incorporate soft and hard tissue grafts to regenerate lost gum and bone tissues.
- Bone surgery (osteoplasty and osteotomy) – Reshapes and smoothes damaged bone to minimize pockets around teeth. May involve bone or tissue grafts.
- Tooth extraction – Removal of unrestorable teeth with extensive periodontal disease. This eliminates sources of infection and inflammation. The swollen gums can then heal.
- Laser gum contouring – Lasers precisely reshape and sculpt gum tissues around teeth for aesthetic purposes or to access dental decay and subgingival margins.
- Dental abscess incision and drainage – Lancing abscesses relieves pressure and infection, combined with antibiotics.
Other Gum Pain Relief Approaches
- Night guards and bite splints – Protect teeth from grinding damage and reduce force on inflamed gums.
- Oral rinses – Prescription antimicrobial or anti-inflammatory rinses aid gum healing.
- Canker sore treatment – Cauterizing, numbing, or removing irritation on mouth ulcers.
Keeping up with professional dental cleanings and following recommended home oral hygiene can help avoid many cases of painful gum disease. But when gum pain flares up, promptly see your dentist to get the proper diagnosis and treatment based on your specific condition for the most effective pain relief and healing.
Home Remedies to Soothe Gum Pain

Along with professional dental care, these self-care tips can temporarily relieve gum pain and inflammation:
Use Soothing Oral Rinses
- Saltwater rinse – Dissolve 1/2 teaspoon salt in a cup of warm water. Swish gently around the gums 2-3 times a day to reduce swelling and keep the area clean.
- Hydrogen peroxide rinse – Dilute with water and swish to disinfect and soothe irritated gums.
- Chamomile tea rinse – Contains natural anti-inflammatory properties to ease gum discomfort.
Take Over-The-Counter Medication
- OTC pain relievers like ibuprofen (Motrin, Advil) or acetaminophen (Tylenol) can ease gum pain. Use as directed.
- Topical numbing medication like Orajel applied directly on the gums temporarily eases pain. Take care not to exceed dosage guidelines.
Adjust Oral Hygiene
- Use extra soft toothbrush – Reduce irritation to inflamed gums.
- Floss extremely gently – Avoid cutting gums further.
- Avoid alcohol or peroxide-based mouthwashes – These can dry and sting irritated gums.
Apply Cold or Heat
- Cold compress – Place an ice pack wrapped in a cloth against the outside of the jaw to minimize inflammation and discomfort. Use for 10-15 minutes at a time.
- Warm compress – A warm wet washcloth may soothe tender gums. Make sure water is not too hot.
Modify Diet
- Stick to soft foods – Avoid spicy, salty, acidic or sugary foods that can further aggravate inflamed gums.
- Drink cold beverages – Very cold water, tea or juices can numb mild gum pain.
These simple self-care measures can provide temporary gum pain relief until you can receive professional dental treatment. They help reduce inflammation and may limit infection spread. However, gum pain persisting more than 1-2 days or any severe symptoms require prompt dentist evaluation and treatment.
When to See a Dentist for Gum Pain
Contact your dentist promptly if you experience any of the following:
- Bleeding or discharge from gums
- Significant swelling in gums
- Pus around gums
- Loose, separating or shifting teeth
- Unusual gum recession or resorption
- Persistent bad taste or mouth odor
- Severe or radiating dental pain
- Gum pain and headaches concurrently
- Slow-healing mouth ulcers or lesions
- Chronic dry mouth symptoms
- Difficulty eating or drinking due to gum sensitivity
Severe, unrelenting gum pain usually indicates infection or advanced periodontal disease requiring urgent dental care. But even mild to moderate gum pain lingering more than a couple days warrants a dental visit to identify the underlying problem and begin appropriate treatment. This can prevent small issues like gingivitis from progressing to advanced gum disease and permanent tooth damage. Prompt care of sudden gum trauma can protect against lasting problems. Don’t delay in seeing your dentist if your gums hurt – healthy gums are vital for the entire mouth.
Preventing Gum Pain

Practicing excellent daily oral hygiene and getting regular professional care protects gum health and reduces the likelihood of painful gum problems. Prevention tips include:
- Brush thoroughly twice a day
- Floss at least once daily
- Use antimicrobial mouth rinses
- Have professional cleanings and exams every 6 months
- Eat a balanced, nutritious diet
- Quit smoking – a major risk factor for gum disease
- Control health conditions like diabetes that increase gum problems
- Drink plenty of water to promote oral health
- Take medications as directed that cause dry mouth or gum growth
- Use night guards if you grind teeth
- Replace missing teeth to prevent
- Visit your dentist at the first sign of gum irritation
The sooner gum disease and other oral infections are detected and treated, the better chance you have of reversing damage and avoiding major surgery or tooth loss. Plus your gums will feel healthier and happier when problems are caught early! Pay close attention to your gum health and take care to prevent issues before they arise.
Answers to Frequently Asked Questions About Gum Pain:
1. What foods should I avoid if I have gum pain?
Avoid foods that are excessively hard, chewy, crunchy, spicy, salty, sour, sugary or acidic when you have gum pain. These types of foods can aggravate inflamed gums. Stick to soft, bland foods and beverages while your gums heal.
2. Can my gum pain be caused by oral cancer?
Gum pain is rarely associated with oral cancer. However, unexplained bleeding, non-healing ulcers, loose teeth or jaw pain along with gum pain should be evaluated promptly by your dentist to check for oral cancer. Your dentist can identify signs and symptoms during an examination.
3. Is gum pain normal during pregnancy?
Mild to moderate gum sensitivity and tenderness is common during pregnancy due to hormonal fluctuations. However, severe or persistent gum pain could indicate pregnancy gingivitis, a gum infection requiring dental treatment. Maintaining excellent oral hygiene habits and getting professional cleanings during pregnancy protects your gums.
4. Why do my gums hurt when I floss?
Healthy gums should not bleed or hurt with gentle flossing. Gum pain when flossing usually indicates some degree of inflammation or infection. Swollen, irritated gums are more prone to flossing discomfort and bleeding. Improving your flossing technique and consistency helps toughen gums. If pain persists, see your dentist to treat any gum disease present.
5. Can gum pain cause a headache or toothache?
Extreme infections like gum abscesses, advanced periodontal disease or dental abscesses can sometimes radiate pain that triggers headaches and toothache. Treating the source of infection and inflammation often resolves related headaches or referred pain. Consult your dentist promptly when experiencing concurrent pain.
Healthy gums are critical for proper tooth function and longevity. Be attentive to gum pain or irritation and seek dental care promptly when needed. Practicing good daily oral hygiene, having regular dental visits and following your dentist’s recommendations can keep your gums comfortable and pain-free. Don’t ignore sore, swollen or bleeding gums – a little prevention and early treatment goes a long way!