Wisdom teeth, also known as third molars, are the last set of molars to erupt in the mouth. They usually emerge between the ages of 17 to 25 years. For some people, wisdom teeth can emerge without any issues and align properly with the existing teeth. But for many others, wisdom teeth often emerge at an angle or get stuck below the gums, leading to a range of problems collectively known as wisdom tooth impaction. Impacted wisdom teeth can damage adjacent teeth and cause infections and cysts. Extracting impacted wisdom teeth is often necessary to prevent more severe complications.
Symptoms of impacted wisdom teeth
Impacted wisdom teeth rarely cause noticeable symptoms initially. As they exert pressure on adjacent teeth and tissues, the following symptoms may appear:
Pain
A dull, throbbing pain around the jaw where the impacted wisdom tooth is located. The pain may be chronic or intermittent initially and worsen over time as the condition aggravates. The pain can range from mild to severe depending on the extent of impaction and infection. It may radiate to the ear, temple and neck on the affected side. Certain triggers like chewing food can aggravate the pain.
Swelling
The area around the impacted wisdom tooth may swell and become tender to touch. Mild swelling may not be visible but can be felt as a raised or enlarged area on palpation. As infection sets in, severe swelling can occur accompanied by redness, making the cheek appear puffed up.
Redness
The gum around the impacted wisdom tooth often becomes red and inflamed, indicating tissue irritation or infection. The redness may be localized to the gum over the wisdom tooth or spread wider if surrounding gums are also involved.
Headache
Constant dull pain from the impacted wisdom teeth can radiate to the temples, causing persistent headaches on the side where impaction has occurred. The headache is usually a throbbing, aching pain that may worsen with chewing or touch.
Difficulty opening mouth
Swelling and spasms around the impacted wisdom teeth can make it difficult to open the mouth fully. Attempting to open the mouth wide may cause significant pain. This also causes difficulty and pain while chewing food.
Bad breath
Partially erupted wisdom teeth create pockets around them that allow food debris and bacteria to accumulate and decay, leading to bad breath or halitosis. The anaerobic bacteria produce foul-smelling compounds that cause persistent bad odor.
Numbness or tingling sensation
Impaction of lower wisdom teeth can irritate the inferior alveolar nerve, causing tingling, numbness or burning sensation in the lower lip, chin, gums, and front teeth on the affected side. This is a warning sign of potential nerve damage.
Sinus issues
The roots of upper wisdom teeth are often close to the maxillary sinus. Impaction can exert pressure on the sinus floor and obstruct the sinus opening called the ostium. This can lead to sinus pressure, congestion, pain and bad odor from infected mucus draining into the mouth.
Damage to nearby teeth
Impacted wisdom teeth put pressure on and can damage the teeth in front of them. This promotes cavities, chipping, fractures, and loosening of the adjacent teeth over time.
Discomfort or difficulty in jaw movements
Chewing, yawning, and wide opening of the mouth may become uncomfortable or painful due to the swollen and inflamed tissues around impacted wisdom teeth.
Severe complications from impacted wisdom teeth

While impacted wisdom teeth may not cause notable symptoms initially, leaving them untreated can lead to following severe complications:
Infection
Impacted wisdom teeth create pockets around them that can harbor bacteria. This can lead to infections like:
- Pericoronitis – bacterial infection of the gum flap or operculum covering the crown of the wisdom tooth.
- Abscesses – Pus-filled pockets around the wisdom tooth due to infection of the associated cyst or gum tissues.
- Cellulitis – Bacterial infection of the soft tissues surrounding the wisdom tooth.
- Osteomyelitis – Infection of the jaw bone around the wisdom tooth.
- Periodontal disease – Damage to gum and bone structures around adjacent teeth.
Cysts
Fluid-filled sacs called cysts can form around impacted wisdom teeth due to tissue inflammation. The common ones are:
- Dentigerous cyst – Develops around the crown of impacted wisdom teeth.
- Periodontal pocket cyst – Forms in periodontal pockets near wisdom teeth.
- Radicular cyst – Forms at the roots of partially erupted wisdom teeth.
These cysts expand slowly, destroying surrounding teeth and jaw bone.
Tooth decay
Impacted wisdom teeth are hard to clean and allow plaque and bacteria accumulation. This accelerates decay in both the wisdom teeth and the adjacent second molars. Cavities and root decay can develop which may require fillings or root canal treatment.
Damage to other teeth
The pressure exerted by impacted wisdom teeth can gradually damage the root structure and supporting bone of nearby teeth. This can cause gum recession, loose teeth, bite changes, or complete tooth loss over time.
Bone loss
Impacted wisdom teeth destroy some of the jawbone surrounding them as they try to forcefully erupt. Loss of jawbone structure can also occur from cysts or chronic infections associated with impacted wisdom teeth.
Nerve disturbances
Wisdom teeth pushing against nerves can lead to tingling, numbness, or neuropathic pain in the lip, chin, gums, and tongue which may last for weeks after extraction. Rarely, it can cause permanent nerve damage.
Oral cancer
Though rare, long-standing impacted wisdom teeth with chronic irritation increase the risk of cancerous growths in the surrounding tissues and bone.
Systemic infection
Infected wisdom teeth can very rarely spread infection to other parts of the body through the bloodstream, potentially leading to sepsis, especially in immunocompromised individuals.
Who is at risk for wisdom tooth impaction?

Some of the factors that increase the likelihood of wisdom tooth impaction include:
- Insufficient space in the jawbone – Lack of adequate space in the jawbone for the wisdom teeth to emerge properly or lack of space due to already crowded teeth increases impaction risk.
- Misaligned teeth – Crooked, overlapped or misaligned teeth can obstruct wisdom teeth from erupting normally and cause impaction.
- Jaw size – Smaller jawbones predispose to crowding and lack of space for wisdom teeth.
- Abnormal positioning of wisdom teeth – Wisdom teeth angled too far forwards, backwards or sideways are more likely to become impacted against adjacent teeth.
- Dense bones and soft tissues – Very dense jawbone and soft gums make it difficult for wisdom teeth to erupt through.
- Genetics – Some ethnic backgrounds and inherited jaw sizes or structures are associated with higher rates of wisdom tooth impactions.
- Age – Wisdom teeth often become impacted in people over 25 years as the jawbones get more dense and their growth is complete. The likelihood of impaction increases with age.
- Existing gum disease or cavities – These increase the risk of infections after wisdom tooth eruption.
Diagnosing impacted wisdom teeth
If wisdom tooth impaction is suspected based on symptoms, dentists use the following approaches to confirm and determine the extent of impaction:
Clinical examination
- Visual examination of the mouth and manual palpation of the jaw and gum areas provide clues about potential impactions.
- Symptoms like swelling, redness, mouth opening difficulty also indicate likely impactions.
- Probing around wisdom teeth will reveal pockets, cavities or soft tissue problems.
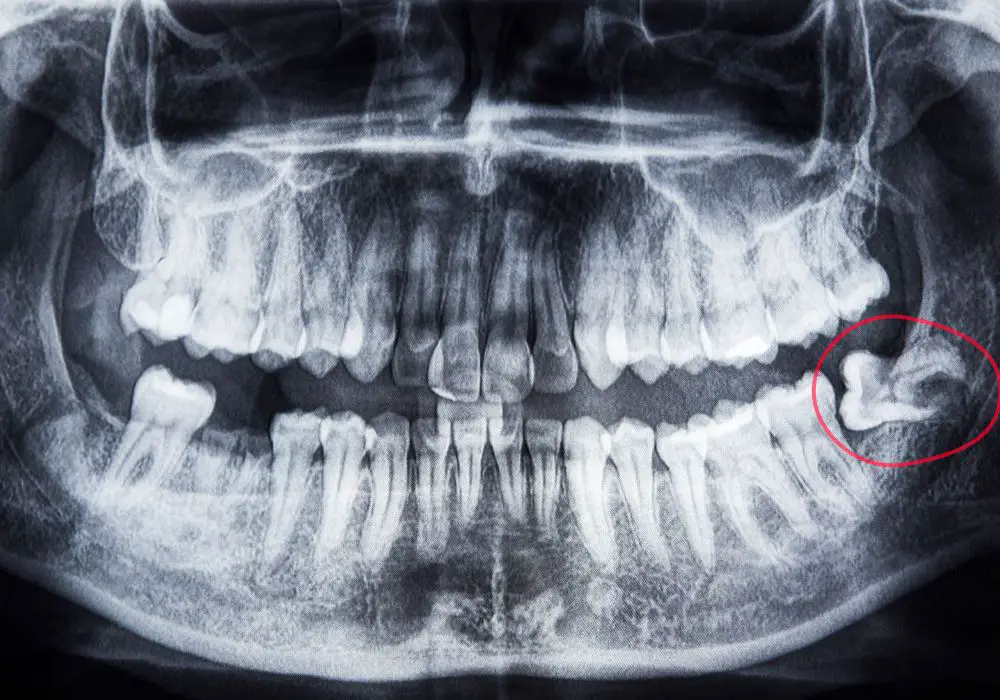
Dental X-rays
- Panoramic x-rays provide a broad view of all teeth, jaws, sinuses, nerves and show the status of wisdom teeth.
- Bitewing x-rays depict incisors to first molars and help detect cavities or bone loss from impacted wisdom teeth.
- Periapical x-rays provide detailed views of individual wisdom teeth roots and surrounding bone.
- Occlusal x-rays show the crowns of upper and lower teeth to visualize impactions.
CT scans
Though not routine, CT scans may be needed to:
- Visualize proximity of impacted wisdom teeth to vital nerves and sinuses.
- Plan surgical extractions when removing teeth near nerves.
- Diagnose cysts or tumors not seen on dental x-rays.
Treating wisdom tooth impaction
Common treatment approaches for impacted wisdom teeth include:
Monitoring
If the impacted wisdom teeth are not causing any symptoms, dentists may decide to just monitor them periodically with x-rays. Monitoring is generally recommended for people over 30-40 years if impactions are stable and high-risk.
Extraction
Surgical extraction of impacted wisdom teeth may be recommended if they are damaging other teeth, causing infections or likely to cause future problems based on position. Based on impaction severity, extraction may be done by:
- A general dentist – For mild impactions with mostly erupted wisdom teeth.
- An oral surgeon – For moderate to severe, difficult impactions where teeth are unerupted, horizontal or pushing on nerves.
Extractions are done under local or general anesthesia. Recovery may take a few days to weeks.
Orthodontic intervention
If wisdom teeth are partially impacted against adjacent teeth, options include:
- Orthodontic treatment to create space and allow wisdom teeth to erupt properly.
- Uprighting or repositioning impacted wisdom teeth so they emerge normally.
- Extracting premolars to create space for impacted wisdom teeth.
Wisdom tooth extractions – Before, during and after

Here is an overview of what to expect with wisdom tooth extractions:
Before extraction
Your dentist will:
- Take dental x-rays to assess impaction. Cone beam CT may be needed to plan surgical extractions.
- Do a clinical exam of the mouth, teeth, and tissues.
- Review medical history, medications, drug allergies, and health conditions.
- Discuss risks, benefits, and alternatives to extraction.
- Recommend extraction if indicated after assessment.
- Give detailed instructions for diet, medication, and preparation needed.
- Prescribe antibiotics or oral rinses to start few days prior to procedure.
- Schedule the extraction procedure.
During extraction
- Anesthesia – Local anesthesia (novocaine shots) or general anesthesia administered.
- Cutting – Incisions made in the gum to expose bone and teeth. Bone or gum may be removed with hand or rotary instruments to access the impacted wisdom tooth.
- Tooth removal – Impacted wisdom tooth is loosened in its socket, may be cut into pieces, and then lifted out carefully.
- Wound cleaning – Socket is irrigated and any debris removed. Bone irregularities smoothed.
- Stitches – The gum incision closed with sutures using absorbable or non-absorbable material.
After extraction
- Swelling, bruising of skin and limited mouth opening are common after effects.
- Medications – Antibiotics, painkillers, mouthwashes may be prescribed.
- Instructions – Diet, oral hygiene, activity recommendations provided.
- Follow-up – Stitches removal and monitoring post-operative healing.
- Healing occurs over weeks to months until extraction site stabilizes.
Wisdom tooth extraction recovery timeline
The recovery period for wisdom tooth extractions varies from weeks to months depending on the severity of impaction and number of teeth removed:
Day of surgery: Swelling, pain, and bleeding from extraction sites are common. Numbness from the anesthesia injection can last a few hours. Significant difficulty opening mouth due to swelling and muscle spasms. Ice application helps reduce swelling. Only liquids or soft foods can be had initially.
First 3 days: Maximum swelling and discomfort during this period as anesthesia wears off. Pain controlled with medication. Jaw stiffness, difficulty eating and speaking persist. Oral antibiotic course started. Head elevation minimizes swelling.
1 week post-op: Swelling, pain and bruising start improving. Able to open mouth wider and with less pain. Still some difficulty eating. Stitches begin dissolving and come out. Oral hygiene with medicated rinses.
2 weeks post-op: Much less pain, stiffness and swelling. Jaw movements start getting back to normal. Able to return to semi-regular diet. Antibiotics and pain meds completed. Salt water rinses help healing.
1 month post-op: Healing nearly complete with minimal pain or swelling. Able to open mouth fully and resume normal diet. Some numbness may remain around extraction sites. X-rays confirm bone healing.
2-3 months post-op: Complete healing achieved in most cases. No pain but may have minor stiffness or numbness near extraction sites that goes away fully over time.
Wisdom tooth extraction recovery tips
Here are some tips to help expedite recovery after wisdom tooth extractions:
- Take prescribed medications (painkillers, antibiotics) on schedule and finish the full course. Stay ahead of the pain.
- Use ice packs on the cheek for the first 48-72 hours to control swelling and improve healing.
- Follow a soft, lukewarm liquid and semi-solid diet like soups, smoothies, mashed foods, yogurt etc.
- Avoid extremely hot, spicy, crunchy, or sticky foods that can irritate the wounds.
- Drink plenty of fluids and avoid using a straw which can dislodge blood clots.
- Gently rinse mouth with warm salt water after 24 hours to keep wounds clean.
- Maintain good oral hygiene using medicated antiseptic mouthwashes as prescribed.
- Sleep with head elevated on 2-3 pillows to prevent swelling and throbbing.
- Take ample rest and avoid strenuous activities for 1-2 weeks after extraction.
- Avoid smoking, drinking alcohol or using tobacco as these delay healing.
- Use OTC pain relievers if needed once prescription pain meds are completed.
- Seek medical help if bleeding, severe pain, pus or fever occur indicating infection.
Wisdom tooth extraction cost with insurance

The cost of wisdom tooth extraction depends on the type of impaction, anesthesia used, number of teeth extracted, and whether it is done by a general dentist or oral surgeon. On average:
- Simple extraction by a dentist – $75-$200 per tooth
- Surgical extraction by oral surgeon – $225-$600 per tooth
- General anesthesia – $150-$400 additional per surgery
Many dental insurance plans cover wisdom tooth extractions but the extent varies. Here is how insurance coverage works:
- Co-pay is typically 20%-50% of the allowed charges.
- Annual deductibles of $50-$150 may need to be paid first.
- Maximum annual dental benefit limits like $1000-$2000 apply.
- Some plans exclude third molar (wisdom tooth) coverage.
- Pre-authorization may be required for surgical extractions.
- Wisdom tooth extraction is covered for adolescents and young adults.
Without insurance, apply for credit care financing if needed. Some dental providers give wisdom tooth extraction discounts for cash payment. Dental schools also offer low-cost options.
Wisdom teeth removal risks and complications
While wisdom tooth extraction is a routine and generally safe dental procedure, some occasional risks and complications include:
Early post-op risks
- Bleeding – Prolonged or excessive bleeding from extraction sockets.
- Pain – Severe pain not adequately controlled with medication.
- Swelling – Excessive swelling and bruising spreading to neck and facial regions.
- Numbness – Prolonged tingling and numbness due to nerve injury.
- Dry socket – Very painful condition when blood clot dislodges from socket.
Late complications
- Infection – Spread of infection to other spaces like cheeks, throat, or bone.
- Sinus problems – Chronic sinus pain or sinus communication opening.
- Nerve injury – Permanent or long-term nerve damage causing numbness.
- Jaw joint issues – Irritation of TMJ or jaw muscles from prolonged opening.
- Bone fragments – Small fractured bone pieces may erupt through gums.
- Damage to other teeth – Usually temporary thermal sensitivity or loosening of adjacent teeth.
However, these complications are uncommon and can be prevented or managed with proper care.
Wisdom teeth removal FAQs
1. At what age should wisdom teeth be removed?
Ideally, wisdom teeth should be extracted when the roots are 2/3rds formed, usually between ages 16 to 24 years. Early removal is easier and prevents impaction.
2. Do wisdom teeth have to be removed?
Not always mandatory. Many wisdom teeth emerge normally without problems. Extraction is advised if impacted or symptomatic based on risk factors. Some dentists also recommend prophylactic removal.
3. How long does wisdom tooth extraction pain last?
Wisdom tooth extraction pain usually peaks on days 2 and 3, diminishes gradually within 1 week, and goes away completely in 10-14 days. Using ice, OTC pain medication, and salt water rinses helps control pain.
4. Can wisdom teeth be removed when pregnant?
Wisdom tooth extractions can be done safely during the second trimester of pregnancy ideally before 24 weeks. Local anesthesia without sedation is preferred over general anesthesia during pregnancy. Any infection should be treated immediately with antibiotics and urgent extraction if required. The procedure should be avoided in high-risk pregnancies.
5. How long after wisdom tooth extraction can I drink alcohol?
You should avoid alcohol for at least 24-48 hours after wisdom tooth extraction as it can interact with pain medications and delay healing. Alcohol causes vasodilation which can increase postoperative bleeding and swelling. It is best to avoid alcohol for a week after extractions.
Conclusion
Impacted or problematic wisdom teeth often need extraction to prevent infections, cysts, decay and damage to adjacent teeth. Though wisdom tooth extraction recovery takes a few weeks, following dentist’s instructions speeds up healing. Good oral hygiene and regular dental care reduces impaction risks. Previously impacted sites must be monitored for potential recurrence. With timely management, wisdom tooth-related problems can be resolved effectively in most cases. However, prevention by early removal remains ideal, especially for high-risk and symptomatic







