The canine teeth, also known as cuspids, eye teeth, or fangs, are the pointed teeth located on each side of the incisors in both the upper and lower jaws. Human canines serve the essential functions of gripping, tearing, and holding food. Their roots give them a stable and resilient anchorage in the jawbone. However, there are times when the removal or extraction of canine teeth becomes necessary for various reasons. This article will take an in-depth look at the key considerations around canine tooth extraction in humans. We will explore the anatomy of canines, reasons for removal, pre-operative preparations, the step-by-step surgical procedures involved, recovery times, aftercare instructions, costs, and potential complications.
Canine Tooth Anatomy
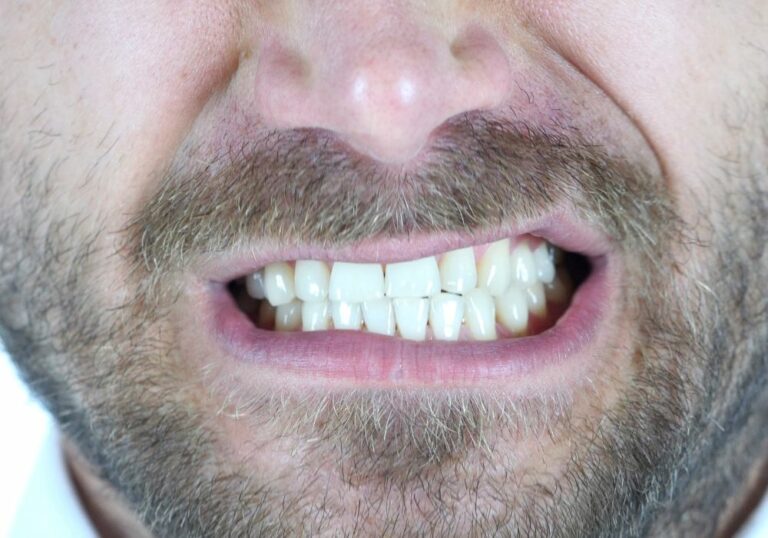
Human canine teeth normally emerge between the ages of 9-12 years. Their conical shape and sharpness help pierce and grasp food. Let’s look closer at the anatomy:
- The visible crown has the longest and sharpest point of all teeth. The tip is called the cusp and is designed to bite and tear.
- Canines have the longest root which anchors them firmly in the jawbone. The single root is generally straight but can be curved in some individuals.
- They are the longest teeth in the mouth after the molars. Upper canines extend below the gum line of the lower teeth when biting.
- The pulp inside contains nerves and blood vessels accessed via the root canal. A layer of dentin surrounds the pulp, topped by tough enamel on the crown.
- A cushion of resilient periodontal ligament fibers attaches each tooth root to the jawbone socket for stable support.
Reasons for Canine Tooth Removal
There are several potential reasons why a dentist may recommend extracting a canine tooth:
Impacted or misaligned canines
Canine teeth that are impacted (obstructed from properly emerging through the gums) or severely misaligned can cause problems like crowding, interference with bite, erosion of neighboring teeth roots, gum disease, and cysts. Removing the affected canine may be the best solution in severe cases to prevent damage.
Fractures
Bad vertical fractures that split the root, or fractures that expose the pulp deeply are often impossible to repair. Extraction is necessary to prevent infection and abscess.
Advanced periodontal disease
Chronic infections around the tooth root can destroy bone, ligaments, and other supporting tissues. Removing affected canines may help stop disease progression and save the other teeth.
Cysts or tumors
Abnormal fluid-filled sacs or benign/malignant tissue growths on canines may necessitate extraction. A biopsy of the removed tooth can determine if the growth was cancerous.
Orthodontic treatment
Extracting protruding, misaligned or blocked-out canines can help create space for movement and alignment of other teeth as part of an orthodontic treatment plan.
Dental prostheses
If a dental bridge, implant, partial denture or crowns are planned, some natural tooth removal may be required to allow proper placement and positioning.
External tooth resorption
A rare condition where the body’s cells essentially attack and begin dissolving tooth structure from the inside out. Extraction is the only fix.
Severe tooth decay/destruction
Deep caries and pulp infection that leaves a canine unrestorable may warrant removal and replacement with a dental implant, bridge or partial denture.
Pre-Procedure Preparation

Diagnosis and treatment planning
The dentist will fully assess the tooth condition through dental x-rays, visual examination, palpation, cold sensitivity testing, and patient history. They will then determine if extraction is the right course of action, discuss options and costs with the patient, and develop an appropriate treatment plan.
Anesthesia options
Since canine removal can be invasive, the dentist will select and administer anesthesia to maximize patient comfort and cooperation. The choices include:
- Local anesthesia – Numbing injections administered around the tooth and into the root tip using lidocaine or similar agents. This is the standard for routine extractions.
- Nitrous oxide – Inhaling this gas through a nose mask produces relaxation and sedation while the patient stays awake. Often combined with local anesthetic.
- Oral sedatives – Anti-anxiety pills and medications like Halcion taken before the procedure.
- IV sedation – Intravenous injection of drugs like midazolam induces a deeper sedation while monitoring vital signs.
- General anesthesia – Total unconscious anesthesia via IV or inhaled gases. Only used for complex surgical extractions.
Managing infection risk
If any tooth or gum infections are present, the dentist may prescribe a course of antibiotics for a few days before and/or after the extraction. This helps prevent bacteria dissemination into the bloodstream during the procedure.
Imaging and impressions
Additional X-rays, CT scans, or 3D imaging may be taken to fully view the roots. Impressions of the teeth may be made to plan any prosthetic replacements.
Canine Tooth Extraction Step-by-Step
There are two main extraction techniques the oral surgeon may utilize depending on the root anatomy:
Simple extraction
This is suitable for canines with relatively straight single roots. It involves:
- Administering local anesthetic to fully numb the area
- Applying forceps or elevators to loosen the tooth and widen the ligament space
- Carefully rocking and wiggling the tooth to detach the remaining ligament fibers
- Slowly pulling the tooth straight out, avoiding cracking the root or socket walls
Surgical (complex) extraction
Curved, hooked, or multiple roots often require:
- Raising a gum tissue flap to access the bone
- Removing supporting bone around the tooth using burs and drills
- Sectioning the tooth with burs if needed to remove hard-to-reach pieces
- Surgically extracting the shards and root tips using elevators and forceps
- Closing the socket and suturing gum tissue back over it
This approach causes more trauma and requires a more involved recovery time.
Post-Extraction Procedures

Controlling bleeding
The dentist will utilize gauze, collagen plugs, sutures, and topical agents to encourage clotting and minimize bleeding after tooth removal.
Debridement
The socket will be irrigated with saline and curetted to remove granulation tissue and infected particles.
Bone grafting
Bone graft material may be placed in the socket to preserve bone volume, especially around front teeth.
Sutures
For surgical extractions, absorbable or non-absorbable sutures close and stabilize the gum flaps.
Medications and instructions
Prescriptions for antibiotics, pain relievers, antimicrobial rinse will be given. Clear post-op directions are provided. Follow-up appointment is scheduled.
Recovery, Healing stages, and Aftercare
With proper aftercare, post-op healing typically progresses through the following stages:
1-3 days: Moderate swelling and pain as anesthesia wears off. Bleeding stops by applying pressure.
3-14 days: Soft tissue healing begins. Take care not to disturb blood clot. Rinse gently after 24 hours.
2-4 weeks: Osseous healing starts as socket begins refilling with bone. Sutures may be removed around day 7-10.
2-4 months: Complete soft tissue closure over socket. Bone completely remodels and reforms.
Long term: Monitor area for abnormal changes indicating complications.
Typical recovery instructions given by dentists:
- Avoid strenuous activity, smoking, and alcohol for 24 hours.
- Use ice packs on face to minimize swelling.
- Take prescribed antibiotics and pain medications as directed.
- Drink liquids and cool, soft foods. Avoid chewing near the site.
- Gently rinse with warm salt water starting 24 hours after.
- Don’t use a straw, spit, or disturb the wound.
- Sleep propped on pillows to reduce throbbing.
- Watch for abnormal or worsening pain, swelling, bleeding, bad taste or fever indicating potential complications.
- Return promptly for all scheduled follow up and suture removal appointments.
With excellent compliance and dental care, the area will heal fully in a few months. Natural tooth replacements can then be considered if desired.
Potential Complications

While not common with proper protocol, potential issues after extraction may include:
- Dry socket – delayed healing and severe pain from natural clot loss. More frequent after lower extractions.
- Post-op infection – due to food debris, poor hygiene, uncontrolled diabetes, or smoking after.
- Bleeding – cysts or anticoagulant use can increase bleeding risk.
- Nerve damage – lingering numbness or altered sensations from injured nerves. Usually temporary.
- Sinus exposure – upper canine roots extending into the sinus can cause a perforation.
Seeking prompt treatment is key if any worrisome symptoms arise after the procedure. Most cases will heal without incident with attentive oral care and follow-up.
Costs of Canine Tooth Extraction
Costs vary based on the complexity of the case, level of sedation needed, insurance coverage, and the dentist’s fees. Average estimates per tooth:
- Simple extraction: $75-$300
- Surgical extraction: $150-$600
- General anesthesia: $200-$500+
Many dental insurance plans cover a portion of extraction costs minus copays and deductibles. CareCredit and other financing options can assist with larger treatment bills.
Conclusion
On occasion, extraction of canine teeth becomes the best option to remedy certain dental health issues and prevent further damage. With modern techniques, anesthesia options, and diligent aftercare, patients can have a smooth procedure and timely healing following canine tooth removal. Close adherence to all post-op instructions and follow-up visits is key to optimal recovery and outcomes. Maintaining ongoing dental health remains vital to keeping natural teeth intact whenever feasible.
Frequently Asked Questions
How painful is canine tooth extraction?
With good numbing anesthesia, most patients report only minor discomfort during the actual procedure. Moderate pain typically occurs in the first 3 days afterward as the anesthesia wears off. Using prescription pain relievers as directed is key to managing post-op discomfort successfully.
Can I still eat after a canine tooth is removed?
Yes, but a soft foods diet is recommended initially. Avoid hot, spicy foods and foods requiring forceful chewing near the extraction site. Drink plenty of fluids. As healing allows, you can gradually return to normal diet in 7-14 days.
Do I need to replace an extracted canine tooth?
It’s not absolutely necessary, but replacement is recommended. Missing canines can shift other teeth, alter bite alignment, increase strain on anchor teeth, and create a gap in your smile. Replacing with an implant, bridge or partial denture restores function and esthetics.
How long after extraction can I get an implant?
Waiting approximately 3-6 months allows adequate time for socket healing before dental implant placement. For complicated cases with extensive infection or multiple extractions, waiting 9-12 months may be better. Follow your surgeon’s advice.
What are signs of a problem after a canine tooth extraction?
Severe pain that increases after several days, excessive bleeding, bad taste, swollen lymph nodes, fever, and redness/pus indicate potential complications like infection or dry socket. Contact your dentist promptly if any worrying symptoms arise.