Wisdom teeth, also known as third molars, are located at the very back of the upper and lower jaws. They are the last teeth to erupt, usually between ages 17 to 25 years. Wisdom teeth have become redundant for modern humans due to reasons including:
- Jaw size – Our jaws have become smaller through evolution while wisdom teeth size remains unchanged. This results in lack of space and impaction.
- Diet – Coarser diets of our ancestors required more chewing teeth. Soft processed foods of today do not require wisdom teeth for chewing function.
- Age of eruption – Delayed emergence increases chances of impaction. Immature root formation in older teens further complicates alignment.
According to research, around 65% of people have at least one impacted wisdom tooth due to lack of sufficient space in the jaws. This often causes problems like pain, infection, cysts, and decay. Thus, wisdom teeth are considered functionless remnants or vestigial structures in our mouths.
Why is the age 17 to 25 years crucial for wisdom teeth eruption?
The late teens and early 20s represent the last stage of jaw development and dental maturation. But this is also a common age for wisdom teeth to cause impaction issues. Some key reasons include:
- Jaws still have residual growth, making room for eruption. Early or delayed emergence limits space.
- Wisdom tooth roots not fully formed, increasing chances of malpositioning.
- Younger soft bone allows easier eruption pathway formation. Dense older bone resists.
- Older patients have higher risk of operative complications.
So this age range is somewhat a transition period between chances of successful or problematic eruption. Dentists closely monitor wisdom tooth status during this time.
How do dentists assess wisdom tooth impaction?
Several methods help reveal the status, position, and potential risks of impacted wisdom teeth:
Clinical examination
Visual and tactile inspection of the teeth and gums to check for swelling, tenderness, infection, cavities etc. Intraoral palpation examines the tooth position below the gums.
Radiographs
- Periapicals – X-rays show wisdom tooth root status and angle of impaction.
- Panoramic – Orthopantomograms reveal wisdom teeth and adjacent structures. CBCT is a more advanced 3D version.
Diagnostic casts
Plaster or digital models of the patient’s dental arches analyze crowding and space availability.
Growth assessment
cephalometric radiographs taken years apart can show jaw growth patterns that indicate future available space.
These diagnostic records help dentists determine the ideal time and technique for management of impacted wisdom teeth tailored to each patient.
How do wisdom teeth affect your bite and other teeth?
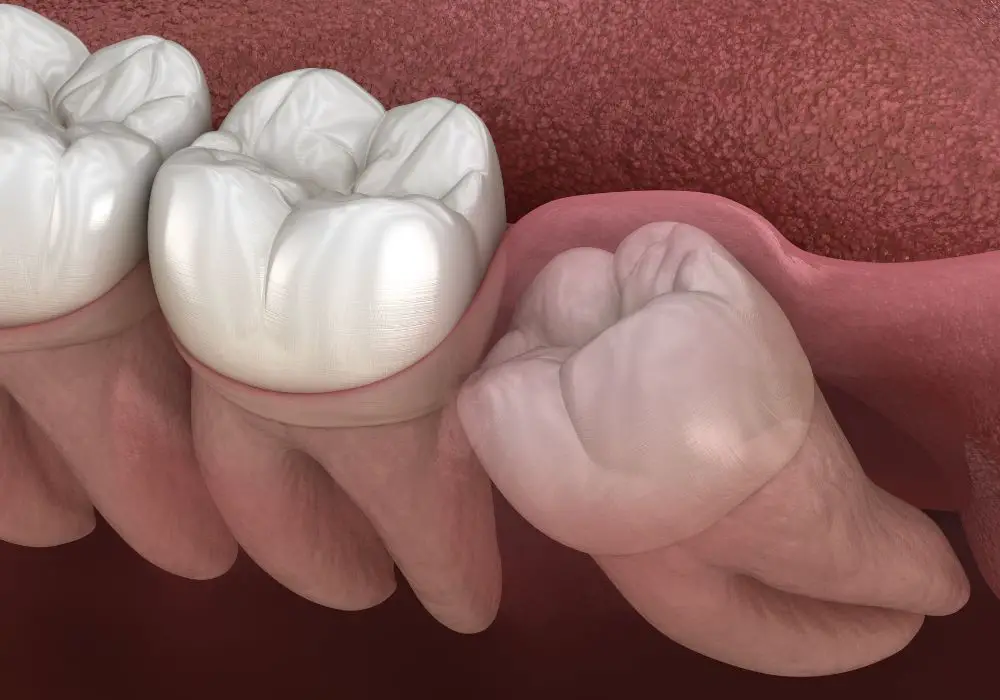
The mesial inclined and compressed position that wisdom teeth frequently get impacted in can lead to various problems:
Crowding and shifting
Impaction exerts forward pressure on the neighboring second molar, progressively pushing it out of position. This sets off a chain reaction causing gradual crowding and misalignment of the anterior teeth.
Occlusion changes
Incomplete emergence due to lack of space can alter the bite relationship between upper and lower teeth. Biting function may be compromised.
Tooth decay and gum disease
The irregular erupted portion of an impacted wisdom tooth traps plaque and debris, increasing decay risk of adjacent teeth. It also causes gum inflammation and pockets around nearby teeth.
Cysts and tumors
Fluid sacs called dentigerous cysts or non-cancerous tumors like odontogenic keratocysts may arise from impacted wisdom tooth follicles. Jaw destruction from expanding cysts can affect other teeth.
Root resorption
Pressure on adjacent teeth, especially lower second molars, can lead to gradual root resorption. This irreversible root structure loss eventually causes tooth destabilization and premature falling out.
When should impacted wisdom teeth be removed?

Due to the potential risks, dentists often recommend prophylactic removal of asymptomatic wisdom teeth in adolescence or early adulthood. However, the ideal timing depends on multiple factors:
- Presence of symptoms
- Type of impaction
- Current damage to adjacent teeth
- Future risk of cavities or cysts
- Jaw development status
- General dental health
Early removal allows for easier recovery and prevents further dental issues. But not all impactions require extraction – some can be monitored if the teeth remain problem-free. Regular dental exams help determine the appropriate treatment.
How are impacted wisdom teeth surgically removed?
Removing impacted wisdom teeth is an outpatient oral surgery procedure performed under local or general anesthesia. It involves making an incision to visualize the tooth and removing bone and tooth structure as necessary to extract it. Some techniques include:
Flap reflection
A mucoperiosteal flap is reflected to expose the wisdom tooth and surrounding bone.
Bone removal
Bone covering impacted teeth is removed with rotary surgical burs or hand instruments to create a path.
Tooth sectioning
Fixated teeth may be sectioned into fragments for easier removal using burs or surgical drills.
Tissue recontouring
Excess soft tissue partially covering the erupting tooth is conservatively excised to aid exposure.
Tooth elevation
Dental elevators are used to carefully loosen and lift out the liberated tooth.
Wound closure
The surgical flap is repositioned back and sutured closed for protective coverage after extraction.
Post-op antibiotics, pain relief, and chlorhexidine oral rinses support recovery after wisdom tooth removal surgery. The dentist later monitors healing and effects on adjacent teeth.
What problems can arise after wisdom tooth removal?
Although relatively safe, certain postoperative complications can sometimes occur after extraction of impacted teeth:
Infection
Pericoronitis, abscesses, and infection of extraction sockets compromise healing. This may require antibiotics and debridement.
Prolonged bleeding
Diffused oozing from the wound is controlled with local hemostatic agents and pressure.
Nerve injury
The inferior alveolar nerve may get bruised or damaged, causing temporary or permanent lip numbness.
Sinus involvement
Removing upper wisdom teeth can accidentally open the maxillary sinus which then gets infected.
Alveolar osteitis
Improper blood clot formation leads to painfully exposed bone known as dry socket syndrome. Medicated dressings provide relief.
TMJ dysfunction
Forced opening and pressure on the jaw joint during surgery can cause transient TMJ pain or bite issues.
Tooth devitalization
Adjacent tooth nerve damage during extraction can require root canal treatment to retain the tooth.
Most postoperative problems are minor and resolve quickly with proper care. More severe complications may need specialized interventions to manage.
Do wisdom teeth hold neighboring teeth in place?
Wisdom teeth are the furthest back teeth, providing no anchorage or stability to other teeth. In fact, impacted wisdom teeth often destabilize the bite by:
- Disrupting optimal jaw growth and development
- Abnormal late growth direction focuses on creating space for wisdom teeth rather than normal function.
- Pushing and tipping adjacent and anterior teeth out of position
- Causing root resorption and premature loosening of nearby teeth
- Reducing periodontal support by harboring infection and decay
However, wisdom teeth do help provide posterior occlusal support, distribute masticatory forces, and maintain the vertical dimension of occlusion. But on balance, impacted wisdom teeth do more harm than good due to associated problems.
What changes can extracting wisdom teeth cause?
Removing wisdom teeth creates space behind the dental arch. This allows adjacent and anterior teeth to gradually drift or tip into the newly available area over months. Some examples include:
- Second molars drift backwards slightly and rotate to occupy the extraction space. This closes residual distal gaps.
- Molars settle together as a unit, reducing arch length. Generalized spacing may decrease.
- Anterior teeth have a mild flaring tendency but this is largely self-limiting.
- Bite collapse or reduction in the vertical dimension is rare since most adjustment happens through tipping movements.
Studies show an average 1.5 mm posterior dental arch width decrease after wisdom tooth removal mostly from second molar mesial drifts. Such minor interdental adjustments are normal and help stabilize occlusion following extractions.
When does shifting become problematic after extractions?
In most healthy individuals, the dental arches compensate well with only subtle drifting and spacing changes after wisdom teeth removal. But certain risk factors can make shifting more pronounced:
- Pre-existing malocclusion or incisor irregularity
- Periodontally compromised dentition with mobile teeth
- Presence of partially erupted or broken wisdom teeth
- Highly aberrant impactions exerting excessive force
- Underlying jaw discrepancies limiting adaptive capacity
- Older age and slower tissue remodeling response
Significant pathologic tooth movement post-extraction can alter function and aesthetics. It may require interventions like orthodontics or prosthetic replacement to correct.
How is pathologic tooth movement managed?

If wisdom tooth removal is deemed necessary in high-risk cases, certain key steps help minimize subsequent shifting:
- Orthodontic treatment – Braces or clear aligner therapy done prior to extraction can consolidate the arches.
- Periodontal therapy – Scaling, curettage, and occlusal adjustment provide a healthy environment for remodeling.
- Tooth stabilization – Splinting mobile teeth for a period avoids drifts.
- Timely replacement – Implants, bridges, or partial dentures replace missing teeth faster to prevent shifting.
- Retention protocol – Clear retainers hold the teeth in place until stabilization.
Regular monitoring and occlusal adjustments are needed to guide the post-extraction teeth to an optimal position. Any problems of bite or spacing are addressed promptly.
Key Takeaways
- Impacted or problematic wisdom teeth commonly affect the health and position of adjacent and anterior teeth.
- Ideal timing for wisdom tooth extraction is late teens when roots are still developing.
- Removing impacted wisdom teeth prevents future problems like cysts, decay, bite issues, and premature tooth loss.
- The dental arch compensates through mild interdental drifts and spacing closure after extractions.
- Severe baseline conditions can cause excessive pathologic shifting which may require interventions to correct.
- Regular dental examinations are key to assessing wisdom tooth status and extraction effects for optimum oral health.
Frequently Asked Questions
Here are some additional commonly asked questions about wisdom teeth extraction effects:
How much shifting occurs after wisdom teeth removal?
On average, minor tooth movements of 1-2 mm occur after wisdom tooth extraction mostly from second molars drifting distally. Limited medial movement of posterior teeth and slight anterior flaring can also occur. Overall positional changes are small and subtle in most people.
Can extracting wisdom teeth cause teeth to become loose or fall out?
Wisdom teeth removal does not directly make other teeth loose or fall out in normal healthy individuals. But pre-existing gum disease, root resorption from impaction, dense bone, excessive force exertion during extraction, or pathological post-op drifting in high risk cases may rarely contribute to loosening or premature tooth loss.
How are gaps closed after wisdom tooth removal?
Gaps distally to the second molars slowly close up over several months due to drifting of the back teeth forwards into the extraction space. This is a natural process requiring no intervention in most cases. If gaps persist due to pathological movement, prosthetic replacement or orthodontic space closure may be needed.
Can wisdom tooth removal shift implants or bridges?
Existing dental implants integrate with bone, so they do not drift or shift position like natural teeth after extractions. However, tooth-supported fixed bridges may develop a poor fit or become temporarily loose if abutment teeth drift significantly. The bridge may need to be re-cemented or replaced for a better fit.
What problems can wisdom tooth removal cause years later?
Wisdom tooth extraction done at the right time and manner rarely causes any adverse long-term effects. But delayed or traumatic surgical technique can lead to late problems like TMJ pain, altered nerve sensations, cyst formation in the bone cavity, periodontal defects distal to the second molars, or aesthetic issues from excessive dental shifting.






