Maintaining good oral hygiene is critical for dental and overall health. However, some individuals seem prone to developing dental problems like tooth decay and gum disease even with regular brushing, flossing, and dental care. This leads to an important question – is bad dental hygiene genetic? Can your genetic makeup and inherited traits predispose you to poor dental health no matter how well you try to care for your teeth and gums? This article takes an in-depth look at the evidence behind the genetic and environmental factors that influence dental hygiene and problems.
Genetic Factors That Affect Dental Hygiene
Tooth Enamel Quality
Tooth enamel is the hard, crystalline mineral outer layer that caps and protects each tooth crown. Enamel is made up mostly of hydroxyapatite crystals organized into rods and interwoven sheets called prisms. The quality and thickness of tooth enamel is determined primarily by genetics and can have a major influence on dental hygiene and susceptibility to problems like cavities.
Some individuals inherit defects in the enamel structure, thickness, and mineral content that make their tooth enamel weaker, thinner, or more prone to chipping and wear. These enamel anomalies are often caused by genetic mutations affecting enamel matrix proteins like amelogenin, enamelin and ameloblastin which are essential for proper enamel formation and maturation. Faulty signaling between ameloblasts (cells that produce enamel) during tooth development can also lead to hypoplastic or hypomineralized enamel.
Thinner enamel with lower mineral content is much more vulnerable to acid dissolution and bacterial enzymatic degradation. Even small defects let bacteria and acids penetrate deeper into teeth rather than being limited to the enamel surface. This leads to rapid decay, sensitivity, and breakdown of the underlying dentin. Enamel defects also cause grooves, pits, and fissures in teeth that are difficult to clean effectively, allowing more plaque to accumulate and colonize with cariogenic bacteria.
Several specific gene mutations associated with inherited enamel defects have been identified, including:
- AMELX mutations – cause X-linked amelogenesis imperfecta, severe enamel hypoplasia
- ENAM mutations – cause autosomal-dominant amelogenesis imperfecta, thin, soft enamel
- MMP20 mutations – cause autosomal recessive hypomaturation amelogenesis imperfecta, enamel lacks mineral content
- KLK4 mutations – cause autosomal recessive hypomaturation amelogenesis imperfecta, enamel is prone to rapid wear and decay
- FAM20A mutations – can cause enamel renal syndrome characterized by kidney defects and thin, soft enamel
The bottom line is that inherited enamel defects negatively impact dental hygiene regardless of how thoroughly someone brushes and flosses. The weakened, defective enamel simply cannot stand up to theroutine wear and acid attacks caused by oral bacteria. This puts sufferers of genetic enamel anomalies at very high risk for rapid decay, tooth loss, and dental problems even with diligent hygiene habits.
Tooth Size and Shape
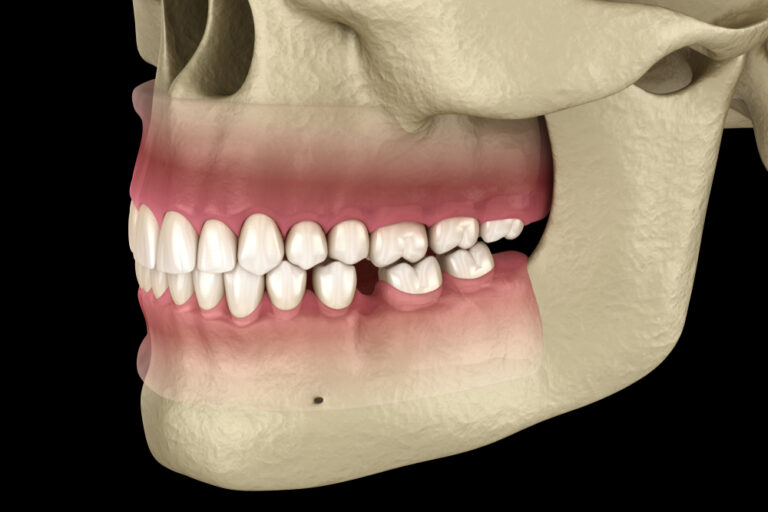
The natural size, spacing, alignment, and shape of teeth are strongly controlled by genetics. Crooked, crowded, or abnormally shaped teeth are more difficult to clean effectively. Food and plaque easily get trapped in hard to reach grooves, narrow gaps between teeth, and areas with improper bite alignment or occlusion.
Smaller upper teeth combined with larger lower teeth, a common dental genetic trait, tends to cause bite misalignment and overcrowding. This is believed to be related to genetic control over relative jaw sizes. Smaller jaws provide inadequate room for the full size adult teeth to erupt properly. Lower teeth may get pushed inward or obstructed by the upper teeth. Conversely, some individuals have teeth too large for their jawbone which also results in crowding and improper alignment.
Tooth shape is also inherited and varies quite a bit among people. Rounded molars with deeper grooves and fissures provide ideal niches for plaque and bacteria to accumulate out of reach of normal brushing. More pronounced dental ridges and cusps also contribute to problems. Pointed canine teeth may overlap other teeth trapping food debris. Even small variations in genetic tooth shape can make cleaning certain areas much more difficult.
Binding studies on twins have estimated the heritability of tooth size and spacing issues to be between 50-80%. While environmental factors play a role, much of the tendency for crooked, crowded, or oddly shaped teeth that are hard to clean is attributable to genetic influences. Such inherited traits directly contribute to increased oral hygiene issues and susceptibility to plaque buildup, tooth decay, and gum disease. Orthodontic treatment can help straighten problem teeth and improve spacing. But teeth want to naturally drift back toward their original inherited positions over time.
Composition of Saliva

Saliva is a crucial fluid for protecting and maintaining oral health. It helps neutralize and buffer acids from plaque bacteria, washes away food debris, and provides antimicrobial compounds and antibodies to prevent overgrowth of harmful microbes. Both the quantity and composition of saliva are greatly affected by a person’s genetic makeup. Reduced saliva flow or alterations in critical components of saliva can impair dental hygiene even if brushing and flossing frequently.
The quantity of saliva production is influenced by genes controlling salivary gland structure, nerval stimulation, and hormonal response. Some individuals simply produce lower volumes of saliva which provides less mechanical cleansing of oral bacteria and food particles from tooth surfaces, tongue, gums and cheeks. Dry mouth or xerostomia is a common problem caused by hundreds of medications but also has genetic risk factors.
The proteins and minerals dissolved in saliva also have genetic origins. Low salivary pH and buffering capacity offers less protection from plaque acids that demineralize enamel. Important salivary enzymes like lysozyme, lactoperoxidase, and lactoferrin which inhibit bacterial growth and metabolism are coded genetically. Their antimicrobial activity and concentration in saliva varies between individuals based on genetic differences. Immunoglobulins and other antibodies in saliva that target specific pathogens are also produced genetically.
Certain salivary proteins directly interact with tooth enamel surfaces and oral bacteria, influencing dental hygiene. Mucin glycoproteins lubricate and adhere to teeth, limiting bacterial attachment. Proline-rich proteins bind to tooth mineral helping form the acquired pellicle protective film. Histatins have antimicrobial properties that control plaque but levels vary genetically. Lower concentrations of such key salivary proteins likely increase caries and periodontal disease risk regardless of oral hygiene habits.
Research has shown that variations in salivary proteins like mucins, amylase, and proline-rich proteins are strongly genetically determined. Mutations affecting salivary gland cell function and ductal transport can alter saliva composition and protection against dental disease. In the end, compromised quantity or quality of saliva from genetic factors sabotages even the most diligent oral hygiene practices.
Oral Microbiome Composition
The oral microbiome consists of the incredibly diverse community of over 700 species of bacteria, viruses, fungi and other microorganisms inhabiting the mouth. Research has shown that the composition and ratios of these microbes, both good and bad, is influenced partly by genetics. Differences in oral microbiomes based on genetic variations helps explain why some people seem innately prone to high levels of cavities or gum disease despite careful brushing and flossing.
Studies of the oral microbiomes in twins has estimated that genetics accounts for about 30% of composition variation between individuals. Factors like enamel defects, tooth crowding, and saliva chemistry help determine what oral bacteria can thrive best in any given mouth. The more out of balance the oral microbial community, the more potential for dental hygiene issues and tooth decay or periodontal disease.
Some mouths harbor higher proportions of acid-producing and inflammatory bacteria that damage teeth and gums even with frequent plaque removal. These include Streptococcus mutans, Lactobacillus, Actinomyces, Prevotella, and Porphyromonas bacteria. Elevated levels of such pathogenic microbes seem linked to a genetic predisposition for poor dental health regardless of oral hygiene diligence.
Conversely, protective oral bacteria produce alkali to neutralize acids and antimicrobial compounds to keep pathogens in check. Strains like Streptococcus sanguinis, Streptococcus salivarius, and Streptococcus gordonii help maintain healthy microbial homeostasis. Lower natural levels of these beneficial bacteria in some individuals based on genetic variance and the oral environment also correlate with increased dental problems.
In the future, genetic testing of oral microbiomes may help predict individual disease risk and determine the most effective probiotics and targeted antibacterial therapies to restore optimal oral bacterial balance.
Environmental Factors That Affect Dental Hygiene

Oral Hygiene Habits
While genetic influences play a significant role, maintaining good daily oral hygiene habits remains the single most important factor under personal control for preventing and minimizing dental problems. Diligent oral care cannot fully overcome genetic risk factors, but is critical for limiting dental plaque and controlling oral bacteria to the lowest possible levels.
Regular effective tooth brushing and interdental cleaning with floss or other aids physically removes the dental plaque biofilm and food particles that feed the harmful bacteria which cause cavities and gum inflammation. Brushing ideally should occur twice per day or at minimum once per day. Proper brushing technique that cleans all tooth surfaces for at least 2 minutes is key for plaque removal rather than just briefly going through the motions.
Flossing once per day removes plaque from between teeth and just below the gumline where toothbrush bristles cannot reach. Rinsing out the mouth and cleaning the tongue, cheeks, and gums also helps lower the bacterial load. Avoiding frequent snacking with long periods between eating/drinking allows saliva flow to naturally wash away more food debris and neutralize acids.
For those with genetic risk factors for poor dental health, meticulous daily hygiene is even more crucial to try to compensate and prevent rapid dental deterioration. While genetics are not totally destiny when it comes to oral health, skimping on careful brushing and flossing has even more devastating consequences for the genetically susceptible.
Fluoride Exposure
Topical fluoride strengthens enamel against acid dissolution and decay by incorporating into hydroxyapatite crystals as fluorapatite. Fluoride promotes enamel remineralization and makes it more acid-resistant. Frequent exposure to low levels of fluoride is especially protective. Fluoride washes over tooth surfaces removing some demineralized enamel and redepositing mineral.
Fluoridated drinking water provides a constant low level of fluoride exposure that protects developing enamel against caries and also boosts remineralization and repair of early decay in adults. Over 75% of the U.S. population receives fluoridated drinking water with optimal levels between 0.7 to 1.2 ppm fluoride.
Using fluoridated toothpaste 2-3 times per day ensures additional topical enamel exposure to fluoride with brushing. High fluoride prescription pastes, gels, rinses and varnishes are also available. For those with high genetic susceptibility to rampant decay, maximizing topical fluoride is a must to strengthen vulnerable enamel. Professional topical fluoride applications in the dental office 2-4 times per year provide concentrated preventive benefits.
Avoiding fluoride exposure where possible significantly worsens dental health overall, but especially for the genetically predisposed. Supplemental fluoride can help offset weak enamel, poor saliva, and high cariogenic bacteria levels inherited genetically that sabotage even diligent hygiene.
Access to Professional Dental Care
While daily personal oral hygiene is essential, it has limitations for fully controlling plaque and cannot resolve emerging dental problems. Regular professional cleanings and exams allow meticulous supragingival and subgingival plaque and hardened calculus removal not possible with daily homecare. Dental visits every 6 months ensure emerging decay and gum infections can be detected early and treated minimally before extensive damage occurs.
Catching problems early optimizes chances of reversing issues like gingivitis (early gum inflammation) through thorough professional cleaning and oral hygiene instruction. Once gum disease progresses to advanced periodontitis with significant bone loss, treatment becomes much more difficult.
Poor access to regular dental care allows calculus deposits and dental plaque biofilm to spread and thicken. Oral infections and decay then flourish, especially in those with genetic risk factors or other dental challenges. Restorative care of damaged, broken, or decayed teeth also helps protect oral health. Keeping up with dental visits, even when expensive or inconvenient, helps mitigate the negative impacts of genetic risk for all individuals.
Medications That Reduce Saliva Flow

Hundreds of common prescription and OTC medications reduce saliva production as a side effect, increasing caries risk regardless of genetic susceptibility. With less saliva washing away food debris and neutralizing acids, decay-causing oral bacteria flourish. Dry mouth bacteria also tend to be more acidogenic.
Some major drug categories known to cause xerostomia (dry mouth) include:
- Antihistamines/decongestants
- Antidepressants
- Anti-anxiety medications
- Muscle relaxants
- High blood pressure medications
- Diuretics
- Pain relievers
- Anti-seizure medications
This drug-induced dry mouth creates an oral environment conducive to rapid plaque buildup and tooth decay even with dedicated oral hygiene efforts. Using saliva substitutes, chewing gum, or sipping water to combat dry mouth from medications is important for limiting dental damage.
Gingival Overgrowth from Medications
Some medications promote overgrowth of gingival (gum) tissues which provides even more area for increased plaque accumulation. This inflamed, enlarged gum tissue is more difficult to keep clean. Medications that can cause this gingival hyperplasia include:
- Calcium channel blockers (blood pressure medications)
- Oral contraceptives with progesterone
- Immunosuppressant drugs
- Anticonvulsants (seizure medications)
Meticulous daily oral hygiene and professional cleanings are critical for minimizing gingival overgrowth from medications. Switching drugs may help if possible. Ensuring thorough brushing and flossing to reduce plaque on enlarged gum tissues is key to prevent rampant decay and periodontal infections.
Chronic Medical Conditions
Poorly controlled chronic medical conditions often worsen oral health even with good hygiene due to their inflammatory and immunosuppressive effects. These include:
Diabetes – elevated blood sugar reduces saliva flow, allows gum infections, and impairs healing.
Rheumatoid arthritis – damages periodontal tissues, alters oral microbiome.
Cancer/chemotherapy – increases cavities risk, causes painful mouth sores.
Eating disorders – purging and acid erosion damage enamel.
HIV/AIDS – increases gum disease and fungal/viral oral infections.
Managing medical conditions through medication compliance, lifestyle changes, and diligent professional care is necessary to avoid exacerbating genetic oral health risks. A comprehensive approach addresses how overall health affects the mouth and vice versa.
Unhealthy Diets
Frequent consumption of fermentable carbohydrates and acidic foods/drinks promotes an oral environment conducive to dental problems. Sugars and refined carbohydrates are metabolized by plaque bacteria into enamel-demineralizing acids and provide fuel for bacterial growth. Prolonged acidic conditions in the mouth weaken enamel and inhibit remineralization.
Frequent snacking or sipping on sugary/acidic foods and beverages maintains constantly high levels of plaque acid production. Sticky foods like raisins and candy cling to teeth allowing prolonged acid attacks. Chronic acid erosion from gastric reflux or eating disorders also damages enamel and dentin.
Limiting sugar/acid intake through a whole food, low glycemic diet is beneficial for all individuals but especially critical for offsetting genetic risk factors for poor dental health. Nutrient deficiencies from poor diets can also impact development of strong enamel. Getting sufficient vitamin D, calcium, phosphorus, vitamin K2, and other minerals is necessary for building sound tooth structure less prone to breakdown.
Key Takeaways – The Verdict on Genetics versus Environment

While genetics do play a significant role and create risk for some individuals, environmental and lifestyle factors often have an equal or greater influence on oral hygiene and dental health vs genetics alone. Most genetic risk factors likely arose from limited dental care access and primitive diets historically. Modern society offers more ways to overcome genetic susceptibility.
The best defense against a genetic predisposition for poor oral health involves comprehensive preventive strategies:
- Meticulous daily oral hygiene – brushing, flossing, tongue/gum cleaning
- Regular professional cleanings and exams every 6 months
- Fluoride exposure through water, toothpaste, prescription strength applications
- Avoiding smoking and limiting sugary and acidic foods/drinks
- Managing chronic medical conditions like diabetes that exacerbate oral diseases
- Monitoring for dry mouth and gingival overgrowth from medications
Certain individuals may need to take extra preventive measures like prescription strength fluoride applications or more frequent dental visits if genetic factors like enamel defects or saliva composition predispose them to accelerated dental problems. However, succumbing to rampant decay and gum disease does not have to be inevitable just because of a genetic predisposition.
Work closely with your dentist and hygienist to optimize daily home preventive care and professional treatments based on your specific genetic, medical, and lifestyle risk factors. While genetics related to tooth anatomy, enamel, saliva, and oral bacteria certainly contribute to dental disease risk, daily oral hygiene habits and diet likely play an even bigger role. Be proactive against your genetic odds through diligent oral self-care and professional maintenance.
Frequently Asked Questions
Q1: Is bad breath (halitosis) genetic?
Bad breath is most often caused by oral bacteria populations and food debris rather than genetics. However, an individual’s oral microbiome composition which contributes to odors has some genetic influence. Dry mouth (xerostomia) from reduced saliva flow, which can have a genetic component, also increases bad breath due to bacterial overgrowth. Using mouthwash, brushing and flossing thoroughly, cleaning the tongue, and regular dental visits all help combat bad breath regardless of genetic risks. Staying hydrated and avoiding foods that contribute to odors (garlic, onions, etc) also improves breath.
Q2: Can you be born with weak, defective enamel or dentin?
Yes, several inherited genetic mutations are associated with enamel defects that result in weaker, thinner, or improperly formed enamel. These include amelogenesis imperfecta, enamelin (ENAM) gene mutations, MMP20 defects, KLK4 defects, and FAM20A mutations. The dentin underneath also